Anterior Hip Replacement
What is Total Joint Replacement Surgery?

Total joint replacement surgery is one of the most advanced successful procedures in patients dealing with severe hip and knee pain. The goal of the surgery is to relieve pain and restore the normal functioning of the joint and help patients resume normal activities.
Anterior Hip Replacement
Over the past few years, there have been great advances in the treatment options, implants, and minimally invasive techniques. The latest technique in joint replacement such as anterior hip replacement has resulted in a dramatic improvement in outcome.
What is Direct Anterior Approach Hip Replacement Surgery
Direct Anterior Hip Replacement is a minimally invasive hip surgery to replace the hip joint without cutting through any muscles or tendons. Traditional hip replacement involves cutting major muscles to access the hip joint. Normally, after a traditional hip replacement, your surgeon would give you instructions on hip precautions to allow the cut muscles to heal.
However, for anterior hip replacement patients, hip precautions are not necessary as no muscles are cut.
Advantages of both anterior hip replacements include:
- Less postoperative pain
- Minimal soft-tissue trauma
- Smaller incision
- Less scarring
- Minimal blood loss
- Shorter operative time
- Quicker recovery
- Early mobilization
- Less postoperative restrictions
- Quicker return to normal activities
- Short hospital stay
Timeline for Hip Replacement (What to Expect)
-
Dr. Hickman Introduction
-
Arthritis of the Hip
-
Recovery Period for Joint Replacement
-
Hip Replacement Recovery
-
Physical Therapy and Postop Pain Management
Surgery Scheduled with Joshua Hickman, MD
- Review the information about your surgery at joshuahickmanmd.com
- Ensure that you have a preoperative appointment scheduled with Dr. Hickman or the physician assistant 1-3 weeks prior to surgery
- Make a list of all current medications including dosages and times taken and bring this to your preoperative appointment
- Receive primary care physician clearance for surgery if instructed by Dr. Hickman's office
One to Three Weeks Prior to Surgery
- Stop all anti-inflammatory medications (Diclofenac, Naproxen, Ibuprofen, etc.) 1 week before surgery.
- If you are on a blood thinner, contact Dr. Hickman's office or be sure to discuss this at your pre op to determine when it needs to be stopped
- Make sure to attend your preoperative appointment with any questions you may have.
- Notify your physician if you or any family member has a history of previous DVT/blood clot
Day Before Surgery
- The hospital or surgery center will call with instructions and arrival time
- Bring your own loose-fitting clothing for therapy after surgery
- Nothing to eat or drink after midnight
- Bring a list of medications including dosages and instructions to the hospital
- If you use a CPAP machine, bring it with you to the hospital
- Scrub the hip and entire leg with the brush given to you at your preoperative appointment
Day of Surgery
- Upon arrival to the hospital or surgery center, you will have labs drawn and an IV placed
- IV antibiotics will be given 30 minutes prior to surgery to decrease the risk of infection
- You will be given spinal anesthesia (we work to perfect the optimal anesthesia and pain control as well as decrease nausea)
- You will be given minimal sedation to relax and sleep through the surgery but no tube will be placed down your throat, you will breathe on your own during surgery
- Surgery time is approximately 60-90 minutes
- You will be given minimal sedation to relax and sleep through the surgery
- No tube will be placed down your throat. You will breathe on your own during surgery
- We will wear special suits and practice sterile techniques in an effort to prevent infection
- A small incision is made to preserve muscle
- The implant will perfectly match your anatomy and will allow for near normal function and motion
- A bandage and ice will be placed on your hip
- You will be in the recovery room for approximately 45 minutes
- Specialized nurses trained in joint replacement recovery will welcome you to the floor. Our staff takes pride in serving your needs and routinely is ranked at the highest level of quality care
- Your diet will consist of solid foods and you will have several menu choices
- There are typically no restrictions on light to normal activities
- Important Tasks on Day 1:
- Sit up in bed, eat regular food, and drink
- Urinate on your own (if not within 4 hours of arrival on the floor, notify the nurse)
- Deep breathe
- Stand and get out of bed with staff assistance
- Walk the halls with assistance
- IF THESE TASKS ARE ACCOMPLISHED YOU MAY GO HOME THE DAY OF SURGERY, most hip replacement patients go home within 24 hours of surgery
First Day After Surgery
- Your dressing will be changed
- You will have physical therapy in the morning and afternoon
- An occupational therapist will discuss issues such as dressing, driving, getting in and out of vehicles and other helpful home tips
- A discharge planner will meet with you regarding discharge
- You will receive a blood thinner to prevent blood clots and you will need to take as directed
- You will receive pain medication orally in the hospital as well as an IV anti-inflammatory medication
- You will go home with main medication. GET OFF PAIN PILLS as soon as possible. Narcotics will not be refilled after 4-5 weeks postoperatively
- Please notify the staff of any issues with urinating but keep in mind that difficulty with bowel movements is normal (it could be several days before you have a bowel movement)
- You will receive instructions regarding your incision, medications, and bathing before you leave the hospital
1-3 Weeks After Surgery
- You should not have a dressing, you may cover your incision with sterile gauze and light tape if spots or small amounts of drainage occur (this is common)
- You may get your incision wet with soap and water, but don't soak it
- Peel off tape strips and clean incision 2 weeks after surgery
- No hot tubs or under-water baths for 4 weeks
- Most hip replacement patients do not need outpatient physical therapy
- Walk frequently throughout the day followed by ice and elevation
- Most patients will not have restrictions on normal activity, participate in activities as tolerated
- Fever around 100 degrees in the first week is normal
- It is common to have bowel difficulty, however, notify our office if you go several days after leaving the hospital without a bowel movement
- Some bruising, swelling, and redness is normal
- It is common to have some numbness around the incision
- Worrisome findings include: drainage from the wound, redness that increases, shortness of breath or chest pain, fever of 102 or higher, and dramatic new leg swelling- contact Dr. Hickman's office immediately if you have any of these symptoms.
- If you have any concerns call 801-295-7200 ext. 112 or email ma.hickman@mountainortho.com
- If you go to a rehab center, you should not stay longer than 14 days
3-6 Weeks After Surgery
- Many hip replacement patients are walking normal or very well without crutches by 3 weeks
- It is common to be stiff and sore at the end of the day
- It is common to be stiff after sitting
- Most patients may continue taking anti-inflammatories as needed (as long as you are cleared to do so by your primary care physician)
- Most hip replacement patients do not need pain pills at all after 3-4 weeks postoperatively
- You should need less and less pain medication and be completely off by week 4.
- There are no restrictions on activity for most patients, in fact increasing your activities as tolerated is good for your recovery
- Worrisome findings include: drainage from wound, redness that increases, shortness of breath or chest pain, fever of 102 or higher, and dramatic new leg swelling- contact Dr. Hickman's office immediately if you have any of these symptoms
3-4 Months After Surgery
- Most patients are back to full activity with no restrictions or difficulty
- Some patients have stiffness and soreness at the end of the day
- Activity should be near normal and you can increase your activities without any restrictions.
12 Months after Surgery
- Less stiffness, however stiffness can exist
- Sore at the end of the day
- Sleeping should improve
- Swelling should be near normal.
FAQs for Hip Replacement
What happens after I schedule surgery?
Dr. Hickman's medical assistant will schedule your surgery with the facility you and Dr. Hickman has been selected. The M.A will then authorize this procedure with your health insurance company. Please understand that authorization is not a guarantee of payment and it is always a good idea that you check with your insurance company regarding deductibles, copays, and coinsurance responsibilities. You should also have selected a preoperative appointment in our office. This usually takes place 1-2 weeks prior to your surgery date.
How do I prepare for surgery?
Have nothing to eat or drink after midnight the night before your surgery. You should also wash your surgical site with an antibiotic soap (which will be given to you at your preoperative appointment). You do not need to shave over your surgical site, this will be taken care of in the operating room.
What time will my surgery be?
Your surgery time will be set by the hospital or surgical center. They will contact your the last working day before your surgery. They usually call after 1pm. Questions or concerns regarding the time of your surgery should be addressed to the hospital.
Should I stop my medications prior to surgery?
This will be discussed at your preoperative appointment. If you are taking Ibuprofen, Naproxen, or any other anti-inflammatories you will need to stop these one week prior to the surgery. If you are on Plavix or other blood thinners, please contact Dr. Hickman's office to determine when these should be stopped prior to surgery. If you are diabetic DO NOT take your diabetic medication after midnight on the day of surgery. The hospital or surgery center will instruct you which of your home medications you should take the morning of surgery.
How do I care for my wound?
Your incision will be closed with dissolving sutures under the skin. There will be no need to remove any stitches. You will go home with two dressings placed on your incision after surgery. The first is directly on the skin and is a clear mesh strip that should be left on for 2-3 weeks. If the strip starts to peel off, trim the edges. The second is an outer brown surgical bandage. The brown bandage should be left on for at least 1-2 days after surgery. Once your surgical bandage is off it is okay to shower and let your incision get wet. Let soap and water run across the incision. rinse clean and pat dry. Do not soak the incision for at least 4 weeks following surgery (no tub, pool, hot tubs, river, creeks, etc.). If you have any concerns about your incision you can email a picture to ma.hickman@mountainortho.com
How will my wound look after surgery?
Redness and increased warmth around your incision can be normal. You may continue to note increased warmth for up to one year. If you experience significant drainage from your wound (drainage that soaks through a gauze pad in 5-6 hours), redness extending away from your incision or flu like symptoms, please notify our office immediately.
Do I need TED hose (compression stockings)?
Most patients do not need compression stockings after surgery. They do not help prevent blood clots, but may be helpful in reducing swelling for select patients.
Do I need an ice machine after Surgery?
Ice machines can aid in recovery after total hip replacement. Cold Therapy via an intermittent pneumatic compression (IPC) and motorized cold therapy (MCT) machine is very beneficial following a total knee arthroplasty. MCT circulates cold water through a wrap over the injury or surgical site. Some of the benefits of MCT include: decreased postoperative discomfort, swelling, inflammation, and narcotic use, provides a consistent, comfortable and safe temperature for hours, and enables patients to control and self-regulate pain management at home. IPC mimics natural muscle contractions to increase blood flow, oxygen, and mechanically flush edema from the affected site. When combined with cold therapy, IPC has shown to: decrease analgesic drug requirements, improve range of motion (ROM) during post op recovery, provide better pain control and improve post operative recovery. We provide ice machines through our office. Unfortunately, we cannot bill your insurance for this item so it will be an out of pocket expense. Contact Dr. Hickman's office to inquire about purchasing an ice machine.
What about dental work after joint replacement?
All dental appointments should be avoided for the first 3 months following surgery unless in an emergency. Antibiotics before dental work are not necessary unless a tooth is being extracted for an infection or major periodontal procedures such as gum or bone surgery. They are not necessary for cleanings, cavity fillings, tooth crowns, or other routine exams.
How long will I need to take pain medication after surgery?
Get off pain pills as soon as possible. You should anticipate discontinuing your pain medication 1-3 weeks after surgery.
Will I need home health after surgery?
Most patients following hip replacement are able to go home without home health care after surgery. Depending on your personal circumstances, some patients may be released to a rehab center or to home with home healthcare. In either circumstance, it is anticipated that you would complete rehab or home healthcare after 7-14 days.
Will I need physical therapy after surgery?
Hip replacements rarely need formal outpatient physical therapy. Dr. Hickman recommends short frequent walks as the best therapy after your surgery.
I'm having difficulty sleeping after surgery, is this normal?
Yes, many patients complain of insomnia and night pain after surgery. This is very normal. Dr. Hickman does not recommend or prescribe sleeping pills.
How much will I follow up with Dr. Hickman?
Your first postoperative appointment will be 3 weeks after your surgery, then a follow up at 4 months after surgery, and again at 1 year after surgery. Then you will need annual appointments each year. Should you have any questions or concerns outside of those time frames, please contact our office.
Physical Therapy After Total Hip Replacement
Your full recovery from your total hip replacement surgery is going to take several months. This website will help you understand your recovery. Guidelines are included which discuss precautions to protect your new joint, exercises that increase you hip strength, and activities of daily living that will help you become an active partner in your care and recovery.
Guidelines to Protect Your New Hip Joint
Your hip surgery did not involve cutting muscles. Motion is usually improved after surgery. Most patients can place all of their weight on the new hip. Having the hip dislocate or "pop out of socket" is almost unheard of with modern implants and surgical techniques. Because of these advances, we are more relaxed in our hip precautions although you may hear of precautions and restrictions in motion that other surgeons use. Below are Dr. Hickman's general guidelines for the first three weeks to help ease recovery of soft tissues.
- Extremes in motion are discouraged for the first three weeks.
- You may bend past 90 degrees if your elbows are inside your knees. Do not twist or rotate your knee inward as you bend.
- It is okay to cross your legs.
- You may sleep on the side of your new hip while in bed. You may place a pillow between your legs for comfort.
- If you are riding in a car, stop every hour or so and walk around for a few minutes.This will help the circulation in your legs and keep your muscles from stiffening up.
- Check with Dr. Hickman when you can resume driving after your surgery.
- Talk to Dr. Hickman about when sexual activity may be resumed and what positions should be avoided.
Our team will teach you in the hospital to use a walker or crutches before you go home. You will quickly progress to a cane. Some patients may not be allowed to put all their weight on the hip immediately. Dr. Hickman will tell you how much weight you can safely put on your new hip. At your three week checkup, Dr. Hickman will tell you if your hip has healed enough to progress to sports or other activities.
Your balance might be shaky for a while.
- Use handrails on steps.
- Use low-heeled or flat shoes.
- Avoid wet or waxed floors.
- Keep your floors free of items that could trip you. Throw rugs or small objects should be kept off of the floor for your safety.
- Watch for pets or other animals that could get in your way.
- Avoid ice or snow.
Adaptive Equipment After Total Hip Replacement
Most patients do not require aids postoperatively, but you patients may benefit from several devices to make your daily activities easier and safer. As your soft tissues heal (though preserved they are irritated), these devices may make certain activities more comfortable. Dr. Hickman and your physical therapist will recommend the equipment that best suits your needs.

Seat / Shower Bench: This seat allows you to sit while bathing and provides you safety while you are in the shower.
Seat Cushion: Cushions are used to elevate the seat height of a chair, couch, car, or other surfaces.

Elevated Toilet Seat: This device is attached to your toilet seat to elevate its height.

Reacher: A reacher is used to pick up items off the floor and help you with dressing.
Dressing Stick: This device has a hook on one end and a pusher on the other end. It is used to help put on pants, skirts, pull up zippers, etc.
Sock Aid: This aid helps you safely put on your sock.

Long-handed Bath Sponge: This sponge helps you clean hard to reach areas while bathing.
Long-Handled Shoe Horn: This shoe horn is attached to long stick and allows you to put on your shoes while sitting or standing.
Managing Activities of Daily Living Following Surgery
Walking with Crutches
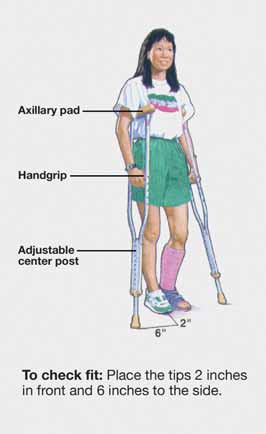
Crutch Safety
- The pressure or weight goes on your hands and not on your armpits. Nerve damage can result if weight is placed on the armpits for a long period of time.
- Keep your elbows close to your side to help keep the crutches against your ribs.
- Your crutch tips should be 2 to 3 inches out to the side of your feet so you do not trip on your crutches
- There should be a slight bend in your elbow when holding onto the crutches (15 to 20 degrees).
- Take your time and do not try to walk too fast.
- Keep your head up and look ahead. Do not look at your feet when walking.
- When walking on carpet, you must pick up your crutches and injured leg more than when you walk on tile or linoleum floors.
- Remove all throw rugs from the floor to keep from slipping and falling.
You may place as much weight on your operated leg as you can tolerate, if told so by Dr. Hickman. Use the crutches to improve your balance and safety, as well as to favor the operated leg when it is painful. Always use a handrail if one is available for stairs and curbs.

Going up with Handrail
- Place both crutches under your arm on the injured side.
- Grasp the handrail with your other hand, if possible.
- Bring your good leg up to the next step. Let the injured leg trail behind.
- Straighten your good leg and bring the crutches and injured leg up.

Going Up without Handrail
- Keep the crutches on the stair you are standing on.
- Support your weight between your crutches.
- Bring your good leg up to the next step. Let your injured leg trail behind.
- Straighten your good leg and bring the crutches and injured leg up.
Going Down with Handrail
- Put the crutch on the lower step.
- Lower your injured leg down to the lower step.
- Support your weight between your crutch and handrail.
- Move your good foot to the lower step
- Put the crutches on the lower step.
- Support your weight between your crutches.
- Bring your injured leg down to the lower step. Let your good leg trail behind.
- Bring your good leg down.
Chair Transfer
Avoid recliners and soft couches until otherwise told by Dr. Hickman. Stiff-backed chairs with armrests are ideal to sit in. If the seat is low, you may place 1 or 2 pillows in the chair to elevate the seat and facilitate transfers



- Back up to the chair until you feel both Iegs touching the chair.
- Slide your operated leg out in front of you as you reach back with one hand for an armrest.
- Lower yourself slowly, keeping your operated leg straight out. Once seated, bend your knee comfortably, or keep it straight.
- When getting up, scoot your operated leg out in front of you.
- Push up using the armrests, keeping your operated leg out in front of you.
Car Transfers
The front seat is preferable because it generally has more leg room, can be adjusted for comfort, and can allow the rider to more easily wear a seat belt.


- Make sure the seat is as far back as possible. Back up to the car with your walker or crutches. Put your operated leg out in front of you.
- Lower yourself slowly to the seat. You may roll the window down and use the car doorframe, along with the headrest, to support yourself as you sit.
- Scoot back into the seat, then swing your legs into the car. If the seat is low, recline the back slightly or put a pillow on the seat to sit on.
- To get in the back seat in a semi-reclining position. You will need to use your arms and non-operative leg to scoot yourself back farther onto the seat.
Putting on Pants

- Slip the underwear or pant leg over your operated leg first by lowering the reacher toward the floor by your foot.
- Repeat for your non-operated leg.
- Pull the underwear or pants up over your knees.
- Stand with the walker or crutches and pull the pants or underwear up.
- When undressing, take the pants or underwear off of your non-operated leg first.
Putting on Shoes
Wear slip-on shoes or shoes with Velcro straps so that you will not have to bend over to put the shoes on and tie the laces. If you are having difficulty, use the long-handled shoe horn or reacher to put on and take off your shoes.
Exercises
Most patients after a hip replacement do not require formal physical therapy. Walking is the best exercise after surgery, beginning with short, frequent walks. The day of surgery, the physical therapist will get you out of bed for the first time. The therapist will help you walk with a walker or crutches as you are able. Each day the amount of walking will increase as you can tolerate. Before you go home, the physical therapist will teach you how to climb stairs safely to protect your new hip.
Additional exercise can help you regain the strength in your hips and legs so you can walk more easily. Below are some basic exercises that should be performed until you can do 3 sets of 10 repetitions very easily. Your therapist at the hospital will also review a home exercise program with you before you are discharged.
Ankle Pumps: This strengthens your calf muscles in your lower leg.

- Lie on your back.
- Bend your ankle and pull your foot and toes towards your head.
- Push your foot back down and point your toes away from you as far as possible, like you are pushing on the brake pedal of a car.
- Repeat with both legs 10 times every 2 hours throughout the day.
Quad Setting: This exercise helps your upper leg or thigh muscles.
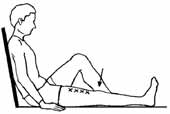
- Tighten the muscles of your thigh.
- Keep your knee straight. Push your knee down into the bed, having your kneecap move upward toward your hip.
- Think about trying to raise your heel ½ inch off the bed.
- Hold for a count of 5 and then relax.
- Repeat with the other leg.
- Alternate legs for 10 repetitions on each side 3 times a day.
Gluteal Setting
- Squeeze your buttocks together. Hold for a count of
- Relax and repeat. Perform a total of 10 repetitions 2 times a day.
Avoiding Problems After Surgery
Blood Clot Prevention: Follow your Dr. Hickman's instructions carefully to minimize the potential of blood clots which can occur during the first several weeks of your recovery. Warning signs of possible blood clots in your leg include:
- Increasing pain in your calf or thigh.
- Tenderness or redness above or below your knee.
- Increasing swelling in your entire leg.
Warning signs that a blood clot has traveled to your lung include:
- Sudden increased shortness of breath.
- Sudden onset of chest pain.
- Localized chest pain with coughing.
Notify Dr. Hickman immediately if you develop any of these signs.
Preventing Infection: The most common causes of infection following total hip replacement surgery are from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your hip replacement and cause an infection.
Following your surgery, you should take antibiotics prior to major dental work or any surgical procedure that could allow bacteria to enter your bloodstream.
Warning signs of a possible hip replacement infection are:
- Persistent fever (higher than 100 degrees orally).
- Shaking chills.
- Increasing redness, tenderness or swelling of the knee wound.
- Drainage from the hip wound.
- Increasing hip pain with both activity and rest.
Notify Dr. Hickman immediately if you develop any of these signs.

